Why Competency Frameworks Are Essential for Fair, Defensible Healthcare Assessment
In healthcare education, assessing students isn’t just about testing what they know. It’s about making sure they’re ready for the real world. That means we need assessment systems that don’t just feel fair, but are fair. So that’s exactly where competency frameworks come in.
Competency frameworks give educators, examiners, and institutions a shared language for defining what “good clinical practice” looks like. Without them, assessment becomes inconsistent, subjective, and nearly impossible to defend.
Let’s break down competency frameworks below. ⬇️
So, What Are Competency Frameworks?
Think of a competency framework as a blueprint for what a learner needs to be able to do by the time they graduate or become licensed. They outline the skills, behaviours, attitudes, and knowledge required for safe and effective clinical practice.
A good competency framework will help answer questions like:
- What exactly should this student be able to demonstrate?
- What does “competent” look like in practice?
- How do we measure performance in a fair and consistent way?
In high-stakes assessments like OSCEs, that clarity is essential.
Why Do Competency Frameworks Matter?
They make assessment fairer
Clear criteria mean examiners know what to look for and students also understand what’s expected.
They strengthen defensibility
If a decision is challenged, you can point to a structured, transparent framework behind the judgement.
They reduce subjectivity
Instead of examiners relying on personal intuition, they assess against agreed and observable behaviours.
They connect the curriculum to assessment
Teaching, learning and assessment become one coherent and aligned system.
They enable meaningful data analytics
When competencies are mapped to assessment scores, institutions can see exactly where learners (or the programme) need support.
Examples of Leading Competency Frameworks
CanMEDS (Canadian Medical Education Directions for Specialists)
Royal College of Physicians and Surgeons of Canada.
Perhaps the most globally recognised model, structured around seven roles: Medical Expert, Communicator, Collaborator, Leader, Health Advocate, Scholar, and Professional.
ACGME (Accreditation Council for Graduate Medical Education)
Core Competencies Guidebook United States.
Six foundational competencies used in residency programmes: Patient Care, Medical Knowledge, Professionalism, Interpersonal & Communication Skills, Systems-Based Practice, and Practice-Based Learning & Improvement.
GMC (General Professional Capabilities)
Outcomes for Graduates – UK.
Defines required outcomes for newly qualified doctors including professional values, communication, clinical skills, and patient safety.
Dublin Descriptors/Bologna Framework
The Bologna Qualifications Framework – Europe.
Broad qualifications framework guiding programme-level outcomes across knowledge, skills, and competencies.
EPAs (Entrustable Professional Activities)
Although this is not necessarily a framework, it is a powerful method for operationalising competencies into real clinical tasks (e.g., “initiate and manage a clinical encounter”). EPAs provide high clarity in workplace assessments.
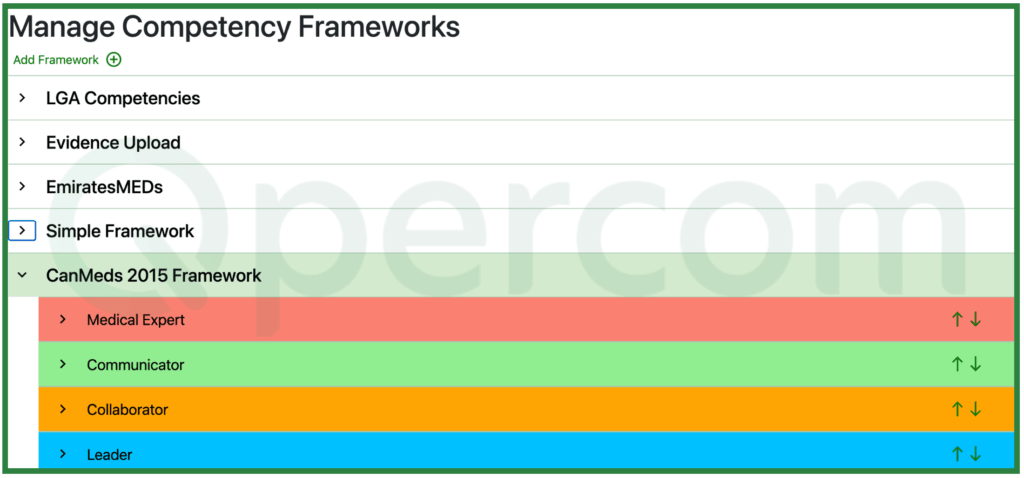
With a good digital scoring platform, competency frameworks can be developed for your specific needs. Qpercom provides a means to add existing frameworks and bespoke models for your assessments allowing flexibility and the ability to create fair, defensible assessments.
Using Competency Frameworks Effectively
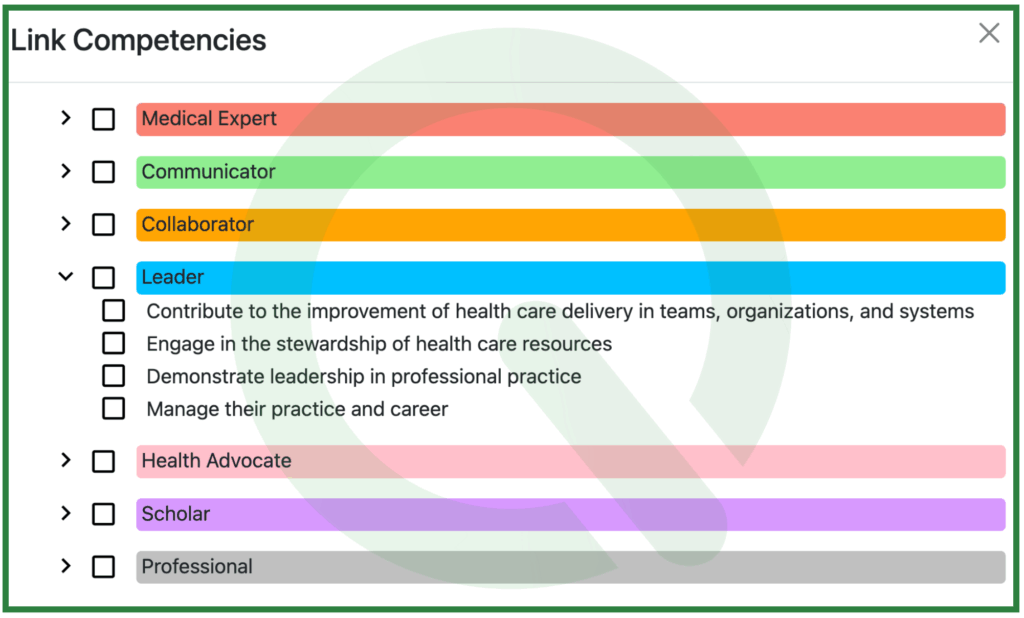
1. Map Competencies to Assessment Items
If a skill matters, it should show up clearly in the OSCE checklist or rating scale.
Qpercom allows competency domains to be tagged to scoresheets and allow sub-domains to be assigned to each question item, giving granular visibility of performance throughout the assessment.
Ensure to make competencies visible inside the assessment itself. Clear mapping ensures your OSCE isn’t just testing isolated skills but genuinely measuring the competencies you claim to teach.
2. Train and Calibrate Examiners
Any competency framework can fall apart if examiners interpret criteria differently. The goal is to shift examiners from judging “how I would do it” to “how the competency describes it”. Effective calibration involves:
- Pre-exam briefings that explain the competencies being assessed.
- Video-based calibration sessions where examiners score sample performances and discuss discrepancies.
- Anchor statements that define what “excellent,” “competent,” and “borderline” look like for each competency.
- Reminders during the exam to stay focused on observable behaviours rather than personal expectations.
3. Balance Your Blueprint
A common mistake is overloading easy-to-measure competencies (communication) and underrepresenting complex ones (clinical reasoning). To balance your assessment:
- Identify which competencies are critical for the exam’s purpose (e.g., patient safety, diagnostic reasoning).
- Build a blueprint that ensures proportional coverage.
- Check that no competency is assessed so rarely that the data becomes unreliable.
- Avoid unintentional bias caused by repeated exposure to certain domains.
4. Keep Teaching and Assessment Aligned
Misalignment between teaching and assessment is a major cause of stress and inconsistent results. Alignment works when:
- Competencies are introduced early in the curriculum.
- Learning outcomes match assessment outcomes.
- Students receive opportunities to practise behaviours linked to each competency.
- Feedback during training uses the competency language they’ll meet in assessments.
5. Analyse Data at the Competency Level
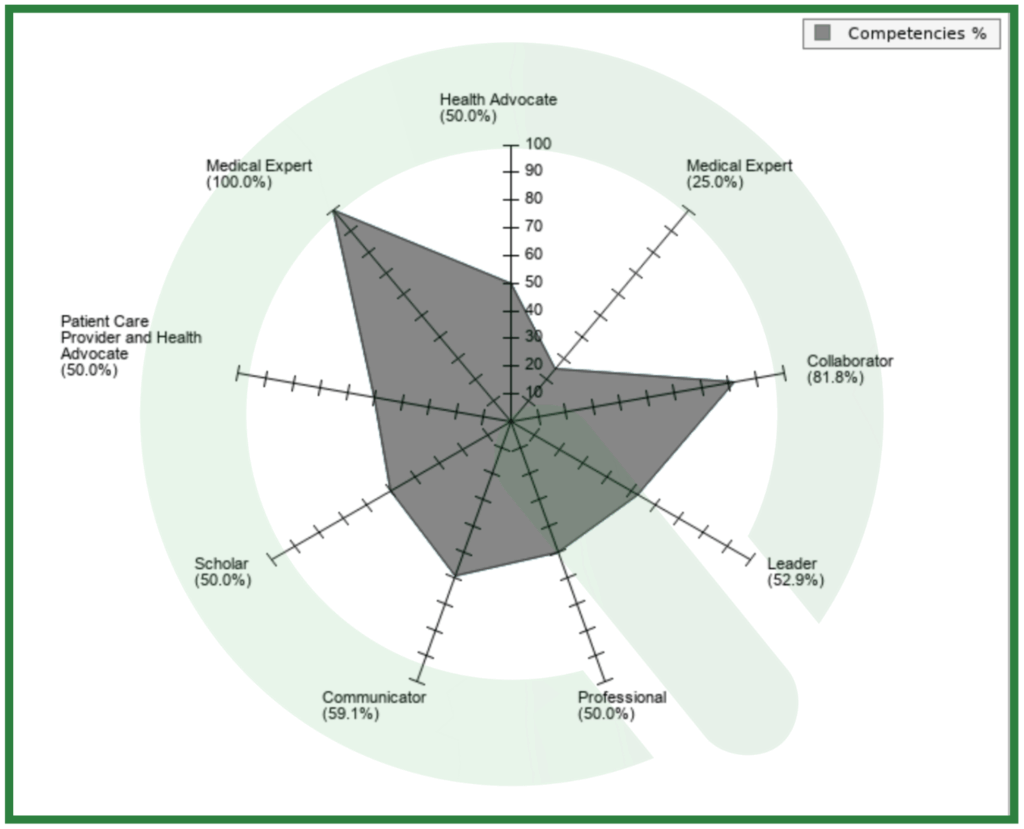
Competency frameworks become truly powerful when combined with meaningful analytics. Looking at results by competency allows you to:
- Identify trends across cohorts (e.g., recurring weaknesses in clinical reasoning).
- Spot issues in station design or examiner behaviour.
- Support remediation with targeted feedback rather than generic scores.
- Provide transparency for accreditation or quality assurance reviews.
- Make high-stakes decisions with confidence, supported by real evidence.
6. Consider Combining Competencies with EPAs
Competencies describe skills and behaviours and EPAs describe real-world tasks. When used together, they create an incredibly rich assessment ecosystem. Here’s how institutions integrate the two:
- Competencies provide the underlying attributes (e.g., communication, professionalism).
- EPAs provide the context (e.g., “conduct a patient consultation”).
- OSCE stations can be designed around EPAs, scored through competencies.
- Workplace assessments can track EPA progression over time.
Final Thoughts: Competency Frameworks Aren’t Optional Anymore
If we want healthcare assessment to be fair, transparent, and defensible, competency frameworks are the backbone. They give structure to what we measure, clarity to what we teach, and confidence to the decisions we make about learner readiness.
They don’t just help students succeed – they protect patients, educators, and institutions.