7 Practical Ways Doctors Can Improve Their Communication Skills
Effective communication is one of the most valuable skills a doctor can master. Whether it’s delivering a diagnosis, providing reassurance, or coordinating care within a multidisciplinary team, communication impacts every aspect of patient experience and clinical effectiveness.
Research consistently shows that doctors who communicate clearly and empathetically improve treatment adherence, patient satisfaction, and even clinical outcomes.1,2 The good news? Communication can be learned, practised, and improved – just like any other clinical skill.3
So… what can doctors do to strengthen this essential skill set, especially in an increasingly digital, fast-paced healthcare environment?
1. Listen More Than You Speak
Listening is essential for building a trustworthy doctor-patient relationship and improving treatment outcomes. It means fully attending to both verbal and nonverbal cues, understanding the patient’s concerns, and considering the impact on their daily life. Doctors can improve listening by creating a comfortable environment, showing interest through body language like leaning forward or maintaining eye contact, using empathetic gestures such as nodding (while being mindful of cultural norms), avoiding interruptions, and asking at the end if the patient would like to add anything further.4 These practices ensure patients feel heard, understood, and respected.
2. Develop Empathy and Emotional Intelligence
Empathy helps doctors connect with the person behind the patient, acknowledging their feelings and perspective without becoming emotionally over-involved. Importantly, empathy is a skill that can be strengthened with training programs and communication workshops that focus on practical, behavioural aspects of empathy.5 Developing emotional intelligence, including the ability to recognise and manage both your own and others’ emotions, further supports effective teamwork, enhances patient relationships, and improves overall satisfaction.
3. Use Plain, Clear Language
In today’s interconnected world, medical professionals serve increasingly diverse populations, and clear communication is more important than ever. Medical jargon can easily confuse or overwhelm patients, so translating complex terms into everyday language, using simple analogies, and checking for understanding are essential.6 By focusing on plain, clear communication, doctors not only make their care more accessible but also uphold their social and ethical responsibility to ensure patients fully understand their health and treatment options.
4. Seek Constructive Feedback
Feedback plays a crucial role in driving professional growth and continuous improvement, especially when it becomes a natural part of clinical practice. Doctors can seek feedback from patients, peers, and supervisors to gain insights into their communication style – focusing on tone, clarity, and empathy, which are often difficult to self-assess. Start by identifying which stage you’re at and setting specific goals for improvement. Be clear about what kind of feedback you’re looking for, and don’t hesitate to ask for clarification if feedback feels too general.7 Building relationships with colleagues and integrating feedback into day-to-day ward activities helps make it a continuous, collaborative process rather than a formal exercise. Remember that feedback is a two-way conversation, not a one-sided critique. When approached as a shared discussion, it fosters mutual understanding, deeper reflection, and meaningful change.
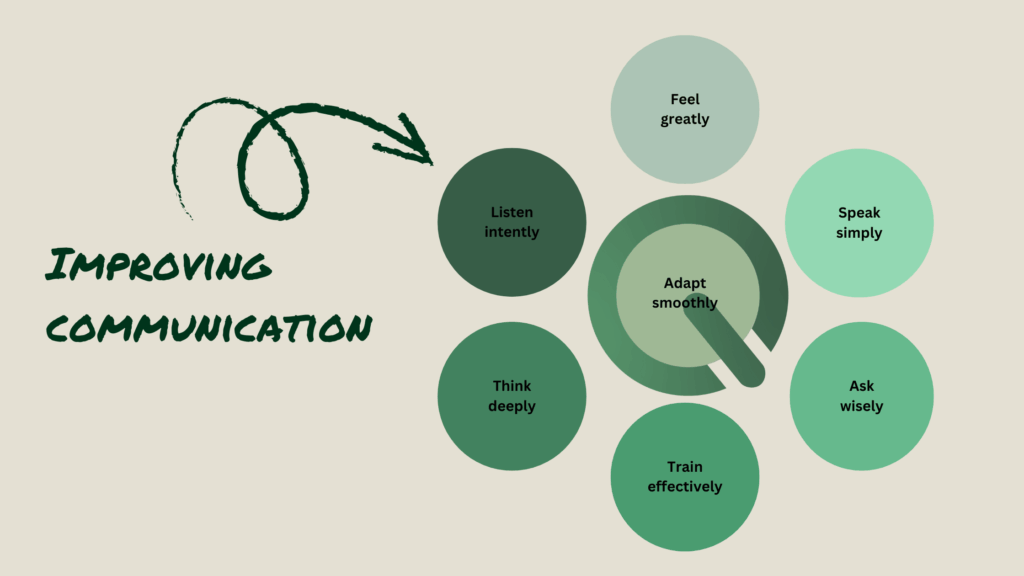
5. Reflect Regularly on Interactions
Reflection turns everyday experiences into valuable learning opportunities and supports ongoing professional growth. For practising doctors, reflection can occur before, during, and after challenging situations which helps to anticipate difficulties and refine responses in real time.8 Among students and trainees, reflective thinking is closely linked with deeper learning and greater meaning-making, even if authentic clinical experience is still developing. Taking time after difficult consultations to consider what went well and what could be improved not only enhances professional development but also strengthens emotional resilience in demanding clinical settings.
6. Train Through Structured Assessments
Communication training shouldn’t stop after medical school. Structured assessments such as Multiple Mini Interviews (MMIs) and Objective Structured Clinical Examinations (OSCEs) allow healthcare professionals to practise communication in realistic, high-stakes scenarios.
Qpercom supports medical schools and healthcare organisations in delivering these assessments efficiently and fairly. With tools for real-time scoring, video review, and psychometric analytics, Qpercom helps educators and examiners identify strengths, ensure consistency, and measure progress in key communication competencies.
7. Adapt to Digital and Virtual Consultations
It’s just as important to practice communication skills for digital and virtual consultations, as they are just as effective as in-person interactions.9 As telemedicine grows, communication must adapt. Doctors should be mindful of tone, body language, and screen presence, as non-verbal cues become harder to read online. Maintaining eye contact via camera and confirming understanding throughout the call are practical ways to ensure clarity and connection in virtual consultations.
Communication isn’t just a soft skill, it’s also a clinical skill. By listening deeply, seeking feedback, and embracing structured assessment and reflection, doctors can continuously improve how they connect with patients and colleagues.
At the end of the day, good communication builds trust, and trust is the foundation of good medicine.