Required Instruments
- Examination lamp.
- Otoscope [Figure 1].
- Ear specula (disposable) [Figure 2].
The Otoscope
An otoscope consists of a rechargeable battery tube [A] and an otoscope head piece [B]. The latter has a contact point [c] for the battery tube. The head piece contains a light source [d], with a retractable, 20 diopter magnifying lens located at the top [e]. At the front end, there is an attachment for the ear speculum [f].
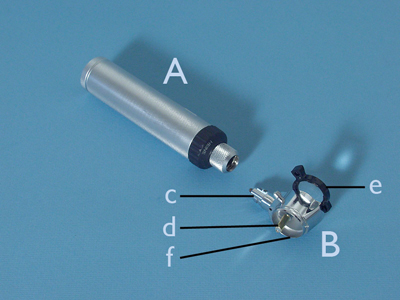 Figure 1
Figure 1
Ear Specula
These are funnel-shaped pieces that attach to the head of the otoscope. At the bottom, they are open. There are different speculae available in various diameters. The indication for the examination determines which diameter is selected. For a regular examination, a tip diameter of 4mm is generally preferred [a]. Sometimes, this is too large when examining infants and young toddlers. A tip diameter of 2mm can then be a solution. For therapeutic procedures that are carried out with use of an otoscope (removal of cerumen, ear wax) a tip diameter of 6mm is often chosen [b].
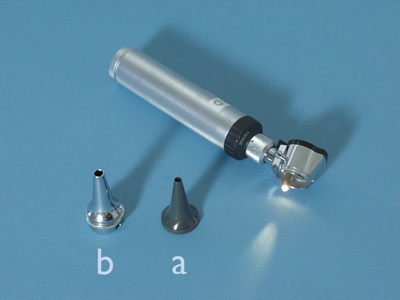 Figure 2
Figure 2
Procedure
- Remain seated next to the patient as for the auricle examination.
- Take the otoscope and attach a clean ear speculum (tip diameter 4mm) [Figures 6, 7].
 Figure 6
Figure 6
 Figure 7
Figure 7
- Take the auricle between thumb and index finger again, and pull it posterosuperiorly in the direction of the crown of the patient’s head.
- To make it easier, rest the other three fingers of that hand on the patient’s head.
- Hold the otoscope in the other hand in a pencil grip.
- The battery tube can point upwards or downwards [Figures 8, 9].
- When the tip of the speculum is positioned in front of the opening of the auditory meatus, look through the lens [Figure 10] and insert the speculum until halfway into the auditory meatus without causing discomfort to the patient.
- The skin that covers the auditory meatus, which will now be in view, should be smooth without any redness.
- It is often covered in a thin layer of cerumen.
- Sometimes, this material is also present in little clumps in the auditory meatus.
- These can vary in colour from yellow-brown to deep red-brown, or even black.
- In some cases, this can close off the auditory meatus completely and the cerumen may even be rock hard.
- If pus is observed in the auditory meatus, you should check whether it is coming from the walls of the auditory meatus or from structures located deeper inside the ear.
 Figure 8
Figure 8
 Figure 9
Figure 9
 Figure 10
Figure 10
- At the end of the auditory meatus, the tympanic membrane can be seen.
- The part that can be observed through the speculum is approximately one-fourth of the total surface area of the tympanic membrane.
- The speculum should be moved carefully inside the auditory meatus to inspect the complete tympanic membrane.
- Caution is required as the wall of the auditory meatus is pain-susceptible, because the skin is quite tightly stretched over the supporting bone and cartilage tissue.
- You should first look for the cone of light.
- This is observed in the anterior lower quadrant of the tympanic membrane.
- Because the tympanic membrane is a conical structure directed inwards and illuminated from a sloping angle, it reflects the light in the shape of a triangle.
- This varies in width, based on the slope of the walls of the funnel.
- The steeper the slope, the narrower the light reflection, the flatter the wall, the wider the light reflection.
- The width of the reflection of the light provides information about the position of the tympanic membrane.
- This is an indication of processes taking place inside the middle ear.
- If there is decreased pressure inside the middle ear because of dysfunction of the Eustachian tube, the tympanic membrane will be pulled inwards, be more conical and the light reflex will be smaller than normal.
- If there is a lot of pus present in the middle ear, the tympanic membrane will be pushed outwards, with the exception of the place where it is attached to the handle of the malleus.
- In such situations, it takes the shape of a halo.
- Because of its convex position, nearly the whole surface will be illuminated diffusely.
- There are also intermediate positions possible between this extreme position and a normal position.
- These give an indication of the degree of excess pressure inside the middle ear.
- When moving the otoscope upwards to the anterior upper quadrant, you will see the thinner Shrapnell’s membrane underneath which the malleus is outlined.
- This membrane also provides information about the position of the tympanic membrane.
- Normally, it lies closely against the tympanic membrane.
- During decreased pressure in the middle ear, the tympanic membrane becomes tightly stretched over this structure; and the malleus protrudes into the auditory meatus.
- During increased pressure, the malleus lies deeper inside the ear than the tympanic membrane.
- Subsequently, move the otoscope towards the posterior upper quadrant and the posterior lower quadrant.
- The colour of the tympanic membrane is usually pearly grey.
- When the tympanic membrane is irritated because of mild inflammation, there may be presence of vessel injection.
- Within severe inflammatory processes, this may lead to the tympanic membrane being bright red in colour.
- If there is a long-term presence of (viscous) mucous effusion in the tympanic cavity, the tympanic membrane can appear yellow-brown or purple-blue in colour due to the substance showing through (glue ear).
- The tympanic membrane can rupture under excessive pressure increase in the middle ear, or through damage incurred from the outside (inserting a sharp item into the ear, cleaning the ear with a cotton bud, sudden loud bangs).
- This is known as a perforation.
- Spontaneous perforations occur most frequently in the anterior upper quadrant.
- When these perforations heal, scar tissue develops.
- Both perforations and scar tissue can impede vibration of the tympanic membrane, thereby giving hearing problems.
- The intactness of the tympanic membrane is therefore an important focal point.
Inspection Of The Tympanic Membrane
A normal tympanic membrane is a thin, transparent structure through which the elements located inside the tympanic cavity can sometimes be visible. Particularly the malleus, the incus and the round window niche can be distinguished. Effusions are detectable in the middle ear because of their colour. Occasionally, air bubbles can be seen in the fluid as well as a fluid level.




























