Procedure
- The patient lies in supine position on the examination table, unless otherwise stated.
- Stand next to the patient and palpate with the tips of the fingers.
- Palpate the skin, Hoffa’s fat pad, the majority of muscles and the patella with the knee in 0° flexion.
- The other structures should preferably be palpated at 90° flexion of the knee [Figure 69].
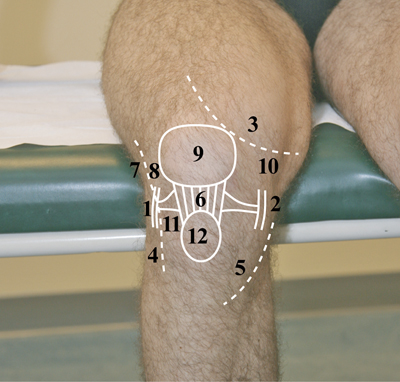 Figure 69: Anatomy Of The Knee At 90 Degrees
Figure 69: Anatomy Of The Knee At 90 Degrees
- Lateral collateral ligament
- Medial collateral ligament
- Contour of the vastus medialis muscle
- Head of the fibula
- Contour of the pes anserinus
- Patellar ligament
- Contour of the iliotibial band
- Lateral femoral condyle
- Patella
- Medial femoral condyle
- Lateral tibial condyle
- Tibial tuberosity
- Ask the patient to indicate exactly when and where they feel pain.
- In the case of an abnormal finding, compare left and right.
- Note:
- Any swelling and characteristics.
- The muscle tone (fingers perpendicular to the course of the fibres).
- The following bones and joints are accessible for palpation:
- Femoral condyles and epicondyles (osteophytic ridges, exostoses, Pellegrini-Stieda syndrome).
- Tibial condyles (osteophytic ridges, exostoses).
- Head of the fibula (fracture, luxation) [Figure 73].
 Figure 73
Figure 73
Patella:
- Inferior pole and superior pole (tendonitis, Sinding-Larsen and Johansson disease).
- Surface (in particular patella bipartita).
- Movement (laterally and medially, proximally and distally).
- Inferior side of the medial and lateral patella for pain (patellar chondropathy) [Figure 70].
- Medial side of the patella (medial retinaculum due to traumatic patellar luxation, presence of a medial plica). The latter can usually be assessed if the patella is slid laterally during palpation.
 Figure 70
Figure 70
Palpation of the base of the patella (right knee). With one hand the patella is slid in a lateral to medial direction during which the medial base of the patella is palpated for pain.
- Medial joint space (meniscus damage).
- Lateral joint space (tenderness in the case of meniscus damage, meniscal cyst).
- The following soft tissues are accessible for palpation:
- Skin (knee region).
- Muscles: In principle, most of the muscles stated in the previous section are accessible for palpation.
- Tendons:
- Superficial pes anserinus [Figure 71] (tendons of the sartorius muscle, gracilis muscle, semitendinosus muscle) and deep pes anserinus (tendon of the semimembranosus muscle).
- Tendon of the biceps femoris muscle; attachment of the iliotibial band to the lateral condyle of the tibia.
 Figure 71
Figure 71
- Ligaments:
- Patellar ligament (jumper’s knee).
- Medial collateral ligament (preferred position: hip in flexion and endorotation, knee in flexion, with the foot flat on the examination table) [Figure 72].
- Lateral collateral ligament (preferred position: hip in flexion and exorotation, knee in flexion) [Figure 73].
Palpation of the lateral collateral ligament. With the right index finger the examiner should palpate the lateral collateral ligament.
 Figure 72
Figure 72
 Figure 73
Figure 73
- Joint capsule (on both sides of the patella).
- Hoffa’s fat pad [Figure 74] (while the knee is extended palpate on both sides of the patellar ligament) (Hoffitis).
 Figure 74
Figure 74
- Bursa (only palpable in the case of pathology):
- Suprapatellar bursa (suprapatellar recess; fluid accumulation; synovial swelling in the case of rheumatoid arthritis, for example; in this case a negative fluid accumulation test is found).
- Prepatellar bursa (housemaid’s knee).
- Infrapatellar bursa (clergyman’s knee).
- Baker’s cyst (medially in the popliteal fossa).
- Nerves: Common peroneal nerve (behind the fibular head).
- Blood vessels: Popliteal artery (in the popliteal fossa).




























