Anatomy and kinesiology
The wrist joint
The radiocarpal joint and the mediocarpal joint are considered to be the wrist joints, and each has its own joint capsule. Movements always take place in both joints.
The possible movements are:
- dorsal flexion (approximately 90°)
- palmar flexion (approximately 80°)
- radial abduction (approximately 50°)
- ulnar abduction (approximately 40°).
In the radiocarpal joint, the distal part of the radius articulates with the scaphoid bone and the lunate bone. Together with the head of the ulna, the distal part of the radius forms the radioulnar joint. Pronation and supination of the lower arm take place in this joint and in the proximal radioulnar joint (from the midpoint position, a movement of approximately 90° is possible for each joint). A triangular fibrocartilagenous articular disc is positioned between the head of the ulna and the triquetrum bone. The base of this disc is attached to the distal part of the radius (distal from the ulnar notch of the radius). The tip radiates into the collagenous connective tissue around the ulnar styloid process. Normally, this disc completely separates the joint cavity of the distal radioulnar joint and the radiocarpal joint.
In the mediocarpal joint, the distal joint facets of the proximal carpal bones (scaphoid, lunate, triquetrum bones) articulate with the proximal joint facets of the distal carpal bones (trapezium, trapezoid, capitate, hamate bones) [Figure 100]. The carpal bones of the proximal row and those of the distal row also articulate with each other. The pisiform bone, together with the ventral side of the triquetrum bone, forms a separate synovial joint.
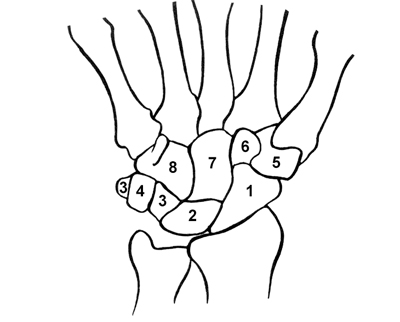 Figure 100
Figure 100
1 scaphoid bone
2 lunate bone
3 triquetrum bone
4 pisiform bone
5 trapezium bone
6 trapezoid bone
7 capitate bone
8 hamate bone
The middle hand
The carpometacarpal joints (CMC joints) are formed by the distal carpal bones (distal hand bones) and the metacarpal bones (middle hand bones). The metacarpal bones also articulate together. Except for in the thumb, the bones in these joints only move very slightly. The metacarpal bone of the 5th digit is capable of slightly greater motion. In the 1st carpometacarpal joint (CMC I) significant movement is possible. This functions as a saddle joint (trapezium bone and the 1st metacarpal bone). The movements that the CMC I joint can make include [Figure 101]:
- flexion
- extension
- abduction
- adduction
 Figure 101
Figure 101
These movements can be tested in combination by asking the patient to alternately carry out opposition (flexion/adduction) and reposition (extension/abduction) of the thumb relative to the other fingers.
The fingers
The joints of the fingers are formed by the metacarpal bones and the proximal phalanges (metacarpophalangeal joints, MCP joints), the proximal and middle phalanges (proximal interphalangeal joints, PIP joints) and the middle and distal phalanges (distal interphalangeal joints, DIP joints). The thumb is an exception. It only has a metacarpophalangeal joint and an interphalangeal joint (IP). The thumb has only two phalanges. The index finger through to the little finger (digits II through to V) can make the following movements:
- MCPs (functionally, in extension position a ball and socket joint, in flexion position a hinge joint):
- flexion (approximately 90°)
- extension (approximately 35°)
- abduction (approximately 20°)
- adduction (approximately 20°)
- rotation (passive)
- PIPs (functionally a hinge joint):
- flexion (approximately 100°)
- extension (approximately 0°)
- DIPs (functionally a hinge joint):
- flexion (approximately 80°)
- extension (approximately 20°)
The thumb (1st digit) movements include:
- MCP I (functionally a hinge joint):
- flexion (approximately 50°)
- extension (approximately 0°)
- abduction (very limited range of motion)
- adduction (very limited range of motion)
- IP (functionally a hinge joint):
- flexion (approximately 90°)
- extension (approximately 20°)
When comparing the movements that the MCP and CMC joints can make, the following observation can be made: the 1st digit is characterised by a high degree of mobility in the CMC joint and limited mobility in the MCP 1 joint. On the other hand, digits II-V are characterised by a high degree of mobility in the MCP joints and limited mobility in the CMC joints.
The most important muscles of the lower arm, wrist and hand
The extrinsic muscles
- brachioradialis muscle
- origin: lateral supracondylar ridge of the humerus
- insertion: directly proximal to the radial styloid process
- extensor carpi radialis longus and brevis muscles
- origin: humeral supracondylar ridge (longus), lateral
- epicondyle (brevis)
- insertion: base of the metacarpal bones II (longus) and III (brevis)
- extensor digitorum muscle
- origin: lateral epicondyle and antebrachial fascia
- insertion: proximal, medial and distal phalanges II through to V
(spreading out into the dorsal aponeurosis of the fingers)
- extensor carpi ulnaris muscle
- origin: lateral epicondyle and antebrachial fascia
- insertion: base of the metacarpal bone V
- flexor carpi radialis muscle
- origin: medial epicondyle and antebrachial fascia
- insertion: base of the metacarpal bones II and III
- flexor carpi ulnaris muscle
- origin: medial epicondyle and antebrachial fascia
- insertion: pisiform bone
- palmaris longus muscle (this is not always present!)
- origin: medial epicondyle and antebrachial fascia
- insertion: palmar aponeurosis
- flexor digitorum superficialis muscle
- origin: medial epicondyle, ulnar tuberosity and anterior radial fascia
- insertion: the sides of the middle phalanges (II through to V) and spreading out into the dorsal aponeurosis
- flexor digitorum profundus muscle
- origin: interosseous membrane, antebrachial fascia and anterior fascia and medial ulna
- insertion: base of the distal phalanges (II through to V)
- extensor pollicis longus muscle
- origin: antebrachial interosseous membrane and posterior ulnar fascia
- insertion: base of the distal phalynx of the thumb
- extensor pollicis brevis muscle
- origin: antebrachial interosseous membrane and posterior radial fascia
- insertion: base of the proximal phalynx of the thumb
- abductor pollicis longus muscle
- origin: antebrachial interosseous membrane posterior radial fascia and posterior ulnar fascia
- insertion: base of the first metacarpal bone
- flexor pollicis longus muscle
- origin: medial epicondyle and anterior radial fascia
- insertion: base of the distal phalynx of the thumb.
The intrinsic musculature
- interosseous palmar/dorsal muscles
- origin: metacarpal bones
- insertion: base of the proximal phalynx (II through to V) and dorsal aponeurosis
- lumbrical muscles
- origin: tendons of the flexor digitorum profundus muscle (2nd through to 5th digit)
- insertion: base of the proximal phalynx (II through to V) and dorsal aponeurosis.
Retinacula, ligaments, tendons and tendon sheaths
The carpal tunnel is a passage located on the palmar side of the wrist which is formed by the carpal bones and transverse carpal ligament (volar) and the flexor retinaculum (the latter two structures cannot be separated from each other as such). Herein lie the tendons of the flexor digitorum profundus and superficialis muscles, the tendon of the flexor pollicus longus muscle and the median nerve. The flexor carpi radialis muscle runs through the wrist but via a different tunnel. The flexor carpi ulnaris muscle also remains outside the carpal tunnel. The palmaris longus muscle is located superficially relative to the flexor retinaculum. In the carpal tunnel, the median nerve is very vulnerable and can become compressed if the pressure inside the carpal tunnel becomes too high. The finger flexors are surrounded by a collective tendon sheath from the transverse carpal ligament onwards. It is often interrupted in the middle hand by the pathway of the 2nd, 3rd and 4th digits. The flexor pollicis longus muscle has its own tendon sheath. Thickening of tendon and tendon sheaths located proximally to the base of the phalanges (‘trigger finger’, ‘snapping thumb’) are common.
The palmaris longus muscle (if present) radiates out into the palmar fascia. Thickening of these fascia can lead to contractures (Dupuytren).
The extensor retinaculum can be found on the dorsal side, in which six tendon sheaths are located for the extensor tendons. These six tendon sheaths each contain their own tendon sheath. One can distinguish between the radial and ulnar side:
- first tendon sheath: tendons of the abductor pollicis longus muscle and the extensor pollicis brevis muscle (De Quervain syndrome!)
- second tendon sheath: tendons of the extensor carpi radialis longus and brevis muscles
- third tendon sheath: tendon of the extensor pollicis longus muscle
- fourth tendon sheath: tendons of the extensor digitorum muscle and of the extensor indicis muscle
- fifth tendon sheath: tendon of the extensor digiti minimi muscle
- sixth tendon sheath: tendon of the extensor carpi ulnaris muscle.
Terminology
Starting position. The hand is placed in pronation and lies in line with the lower arm. An imaginary line can be extrapolated from the third digit through the middle of the lower arm.
Digit. A notional axis through the fingers and metacarpal bones, proximally elongated up to the wrist joint.
Examination technique and sequence
For all examinations you should explain to the patient what you are about to do and you should meet the essential conditions for conducting an examination.




























