General
Normally, examination of the spleen does not provide any positive findings: the spleen is not visible or audible, it yields (almost) no dullness on percussion, and is impalpable. However, disorders involving the spleen can sometimes yield positive results. For example, a ruptured spleen can cause shock, acute abdominal pain (peritoneal irritation), or referred pain (left shoulder pain).
During abdominal percussion, be aware of any dullness across the left costal arch
(Traube’s space) [Figure 30].
 Figure 30
Figure 30
Dullness in this area is indicative of an enlarged spleen (splenomegaly). If this is the case, pay extra attention to investigating the spleen during further examination.
Procedure
Inspection
If splenomegaly is suspected during inspection, check for petechiae (due to thrombocytopenia).
Percussion
- Stand if necessary.
- Percuss along the midaxillary line starting at the left armpit and progressing in a caudal direction [Figures 31, 32], keeping the pleximeter finger parallel to the ribs.
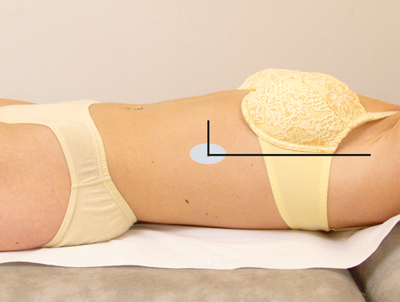 Figure 31
Figure 31
 Figure 32
Figure 32
- The resonant percussion sound heard over the lungs changes to a dull sound at the upper border of the spleen.
- Percuss slightly caudal to this point in a ventral direction [Figure 33] and determine the point at which the dullness changes to the tympanic sound of the abdomen.
 Figure 33
Figure 33
- From the iliac spine, percuss along the midaxillary line in a cranial direction to determine the lower border of the spleen.
- If the spleen appears to be enlarged, determine the extent of the area of dullness, starting from the middle of this area. Indicate this area on a diagram of the body.
Normally, the upper border of the spleen is found at the same level as the ninth rib (in the mid-axillary line).
Ventrally, the dullness normally extends no further than the anterior axillary line. The lower border is in line with the lower edge of the left costal arch. The distance between the upper and lower borders is 4-6 cm at most. Sometimes the spleen is so small that dullness cannot be observed.
If the area of dullness is larger, then splenomegaly is a possibility.
Palpation
Normally, the spleen does not extend beyond the left costal arch and is therefore impalpable. Thus, a clearly palpable spleen always suggests pathology. Palpation of the spleen is only useful if splenomegaly is suspected based on the results of percussion. Palpation of the spleen can be performed while the patient is lying on their back and / or right side.
Procedure
The patient is in supine position:
- Sit to the right of the patient.
- Lay your left hand flat on the left lumbar region parallel to the costal arch
[Figure 34].
If necessary, this hand can be used to exert upward pressure to raise and hold the left side of the thorax in a slightly higher position, which can facilitate palpation.
 Figure 34
Figure 34
- Carefully lay your right hand flat on the upper left abdomen with fingers parallel to the costal arch and index finger caudal to the lower border of the spleen, which has previously been determined by percussion. The fingertips should lie laterally to the rectus abdominis muscle. Generally palpate using the radial side of the right index finger.
- Ask the patient to breathe in deeply and calmly through the mouth.
During inspiration, the spleen is displaced by the contracting diaphragm in a caudal direction. - While the patient breathes in deeply, make a careful gliding motion with the right hand in the cranial direction.
- If the spleen is not felt, repeat this process after repositioning the palpating hand slightly in the cranial direction.
This procedure can also be performed while the patient is lying on their right side with the legs bent slightly at the hips and knees [Figure 35].
In this position, the spleen moves forward slightly, which usually makes it more palpable.
 Figure 35
Figure 35
Focus points
- Use extreme caution when palpating, particularly in cases of splenomegaly.
The gliding movement of the right hand must occur carefully, and the pressure of the palpating fingers should be minimal: an enlarged spleen has a soft consistency, and careless palpation can rupture the spleen. - If the spleen is enlarged, it will be palpable on the radial side of the right index finger while the patient breathes in. A palpable spleen almost always denotes pathology.
In slender patients, the spleen may just be palpable under the left costal arch during inspiration while lying on the right side. - If the spleen is palpable, determine the shape of the spleen by following the lower part of the spleen in both medial and lateral directions, using the methods described above.
If the spleen is palpable, determine the following aspects:- the length in centimetres of the portion of the spleen that extends beyond the left costal arch;
- the consistency of the lower border of the enlarged spleen (varies from soft to firm);
- the quality of the lower border of the enlarged spleen (varies from sharp to blunt);
- palpation tenderness (under normal conditions, the spleen is not painful upon palpation).
- If the spleen cannot be felt while the patient is lying on their back or side, the dullness found during percussion is probably caused by other homogenous structures, such as a filled colon or an intraperitoneal or retroperitoneal mass.




























